Natural Remedies to Help Alleviate Migraine Pain: A Complete Guide
Introduction and Outline: Why Natural Migraine Relief Matters
Migraine is more than a bad headache; it can dim the world, squeeze your focus to a pinhole, and pull the rug from an otherwise ordinary day. Roughly one in seven people worldwide live with migraine, and women are affected more often than men, largely due to hormonal influences. While medications play a crucial role for many, numerous natural strategies can ease pain, reduce frequency, and improve daily function. The aim of this guide is to present practical, evidence-informed tools you can start using today—and to show how small, consistent changes often add up to meaningful relief. Think of this as a field guide: part science, part everyday wisdom, and part gentle nudge toward habits that support a calmer, steadier nervous system. As always, partner with a qualified clinician, especially if you are pregnant, have other medical conditions, or take regular medications.
Here is how this complete guide is organized, so you can jump to what you need most right now:
– Understanding the migraine brain: what’s happening under the hood and why triggers matter
– Everyday foundations: sleep, hydration, nutrition, and movement rhythms that dial down attacks
– Quick relief and natural aids: cold packs, strategic caffeine, herbs, topical oils, and key supplements
– Mind–body methods: breathing, biofeedback, meditation, yoga, and targeted stress skills
– Putting it together: a personalized plan, safety notes, and signs you should seek medical care
Approach this material like tuning a musical instrument. You’ll make small adjustments—timing your meals, focusing your breath, cooling your temples, sipping ginger tea—and notice which notes bring your system back into balance. Keep what works, let go of what doesn’t, and track patterns with a simple diary to inform future choices. Relief rarely arrives via a single magic switch; more often it’s a dimmer, gently turned by a set of steady, doable practices.
Understanding Migraine Biology and Triggers
To choose the right remedies, it helps to understand the puzzle. Migraine involves the trigeminovascular system (nerves that serve the face and head) and a wave of altered brain activity that can heighten pain pathways and sensitivity to light, sound, and motion. Chemical messengers, including calcitonin gene-related peptide (CGRP), play a role in dilating blood vessels and amplifying pain signals. Some people experience aura—visual zigzags, shimmering lights, or tingling—before the headache phase; others never do. The key takeaway is that the “migraine brain” is excitable and sensitive to change. Regularity and gentle stabilization often reduce flare-ups.
Triggers are not causes, but they can tip a sensitive system over its threshold. Common ones include:
– Sleep changes: staying up late, early wakeups, or weekend “jet lag”
– Hormonal shifts: particularly around menstruation, perimenopause, or certain contraceptive changes
– Dehydration and skipped meals: blood sugar dips and low fluid intake stress the system
– Sensory overload: flickering lights, loud environments, strong fragrances
– Weather shifts: rapid barometric pressure drops or heat waves
– Diet patterns: alcohol, aged cheeses, processed meats, and excessive added sugars may provoke attacks in some
– Caffeine swings: both excess and sudden withdrawal can backfire
– Stress fluctuations: it’s often the post-stress “letdown” day that stings
Two people can share a diagnosis yet have entirely different trigger profiles. That’s why a simple log—time of day, sleep the night before, hydration, meals, weather, stress level, and menses—can be so revealing. Over two to four weeks, patterns emerge: maybe late dinners plus screen time after 10 p.m. and a hot morning commute add up to trouble by noon. Having this map allows targeted adjustments. Importantly, triggers stack; a small sleep loss plus mild dehydration and bright office lights together may surpass your threshold even if each alone would not. This is empowering, because lowering just one or two factors can drop you back under the line and prevent an attack from starting.
Everyday Foundations: Sleep, Hydration, Nutrition, and Movement
Natural migraine care starts with rhythms the nervous system can trust. Regular sleep, steady fluids, balanced meals, and modest movement converge to lower attack frequency in many people. These are not glamorous fixes, but like a well-set metronome, they keep the tempo smooth enough to avoid sudden spikes in neural noise.
Sleep: Aim for a consistent window—going to bed and waking within the same 60–90 minutes daily, including weekends. A cool, dark room, a 20–30 minute wind-down, and screens off an hour before bed help set your circadian clock. If you wake at night, gentle breathing and a brief body scan can nudge you back without drama.
Hydration: Even mild dehydration can increase headache susceptibility. As a starting point, many adults do well with roughly 2–3 liters of fluids across the day, more if you sweat heavily or live in a hot climate. Add a pinch of electrolytes (sodium, potassium, magnesium) during long workouts or heat exposure; balanced fluids beat plain water for maintaining stability in those settings.
Nutrition: Focus on regular, not rigid. Skipping meals is a common and preventable trigger. Emphasize protein and fiber at each meal to steady blood sugar. Magnesium-rich foods (pumpkin seeds, almonds, leafy greens), omega-3 sources (fatty fish, walnuts, flax), and colorful produce support an anti-inflammatory pattern. Some find that limiting highly processed foods and rapidly absorbed sugars lowers volatility in headache patterns. If alcohol or certain aged or fermented foods correlate with attacks in your diary, reduce or time them carefully.
Movement: Aerobic activity—like brisk walking or cycling at a conversational pace—three to five times weekly is associated with fewer migraine days over time. Start gently and build: 20–40 minutes on most days is a widely used target. On headache-free days, include mobility or yoga flows that improve neck and shoulder mechanics; tension in these areas often adds fuel to the fire when a trigger hits.
To anchor these foundations, try this simple scaffold:
– Wake, hydrate, light snack if needed, and a 10-minute walk outside
– Regular mealtimes with protein and fiber; avoid long gaps
– Two short movement breaks during work to roll shoulders and relax jaw
– Evening wind-down: dim lights, screen cut-off, and a calming routine
None of this requires perfection. Aim for “mostly consistent,” observe what shifts, and adjust one lever at a time so you can attribute improvements to specific changes.
Quick Relief and Evidence-Informed Natural Aids
When a migraine creeps in, swift, gentle interventions may blunt the rise. Combining a dark, quiet space with targeted cooling, hydration, and a few well-chosen aids can reduce intensity or shorten duration. Think of this as your “go-bag” for flare-ups.
Cold and heat: A flexible cold pack across the forehead or on the back of the neck can constrict vessels and dull pain; some prefer alternating warm compresses on shoulder and neck muscles to melt tension. Try 10–15 minutes, rest, and repeat as needed.
Caffeine: For some, a small, early dose—about 50–150 mg—taken at the first twinge can enhance other strategies. The key is consistency: frequent high doses or late-day use can worsen sleep and provoke rebound headaches. If you are sensitive, consider green tea or simply skip caffeine and lean on other tools.
Topical aromatics: Peppermint or mentholated balms, diluted and dabbed on the temples and neck, show promise for acute relief in small trials. Avoid the eyes and patch-test first. Some also find gentle benefit from lavender oil inhalation during rest.
Ginger: As tea or standardized capsules, ginger appears to support acute relief for some people. A commonly used approach is 250–500 mg of powdered ginger at onset, with a second dose after a few hours if needed, or a strong infusion made from fresh slices. Those with gallstones, bleeding disorders, or who are pregnant should review ginger use with a clinician.
Supplements for prevention: Certain nutrients have a track record for lowering attack frequency when taken daily for several weeks.
– Magnesium: 400–600 mg per day (often citrate or glycinate) may reduce frequency; loose stools are a sign to lower the dose
– Riboflavin (vitamin B2): 400 mg per day is used in several studies; urine may become bright yellow
– Coenzyme Q10: 100–300 mg per day may support mitochondrial energy in sensitive neurons
– Omega-3s: 1–2 g per day of EPA+DHA from food or supplements may reduce inflammatory signaling
Herbal considerations: Feverfew has mixed evidence; some find it helpful, while others do not. It can interact with blood thinners and may cause mouth irritation when used as fresh leaves. Butterbur extracts that are processed to remove pyrrolizidine alkaloids have been studied, but safety concerns persist; many clinicians advise avoiding it due to potential liver toxicity. If you consider any herb, choose reputable sources and discuss with your healthcare professional, especially if pregnant, nursing, or managing chronic conditions.
Acupressure: Gentle pressure on points like LI4 (the web between thumb and index finger) or PC6 (three finger-widths below the wrist crease, inner forearm) for 1–2 minutes per side can ease associated nausea and tension. The technique is safe for most; however, avoid strong pressure if you are pregnant without guidance.
The unifying principle is to act early, combine two or three compatible strategies, and give them 20–40 minutes in a dark, quiet space. If your established rescue plan includes prescription options, these natural steps can complement that regimen—never replace urgent care when red flags are present.
Mind–Body Techniques and Long-Term Nervous System Resilience
Stress itself is not the sole villain; it is the acceleration and braking that jar a sensitive system. Mind–body methods teach your nervous system to downshift smoothly, reducing the peaks and troughs that set off pain pathways. Over weeks to months, these skills can lower attack frequency and increase your sense of control.
Breathwork: Slow, diaphragmatic breathing sends “it’s safe” messages via the vagus nerve. Try the 4-6 pattern: inhale through the nose for 4, exhale for 6, repeat for 5–10 minutes. If you feel dizzy, shorten the sessions until it becomes comfortable.
Mindfulness and meditation: Consistent practice—5–20 minutes most days—can lessen pain-related anxiety and reduce the “threat volume” of early symptoms. A simple anchor is enough: follow the breath, or sweep awareness down the body from scalp to toes. When thoughts drift, return kindly, like guiding a skittish horse back to a path.
Biofeedback: With training tools that mirror back muscle tension or skin temperature, you learn to consciously relax jaw, neck, and shoulder muscles, often reducing attack intensity. Many communities offer structured programs; home devices and app-guided courses are also available. Even without gear, progressive muscle relaxation—tensing and releasing each major muscle group—builds similar awareness.
Yoga and gentle mobility: Slow flows with attention to the neck, upper back, and hips balance muscle tone and restore posture. Emphasize non-straining positions, smooth nasal breathing, and longer exhales. On vulnerable days, opt for restorative poses instead of vigorous sequences.
Cognitive strategies: Simple cognitive-behavioral skills help you unhook from catastrophic loops. Rephrase “this will ruin everything” into “this is uncomfortable, and I have a plan.” Tiny reframes shift physiology more than they seem to; the mind’s lens is a powerful modulator of pain circuits.
Routine micro-doses of calm add up. Consider scheduling brief resets:
– Two-minute breathing practice every 3–4 hours during the workday
– A five-minute shoulder and jaw relaxation before lunch
– A ten-minute restorative pose or walk after work, screens away
– A three-minute gratitude or journaling check-in at bedtime
Over time, these practices become a cushion, so when triggers stack up, your threshold holds higher. They are not instant erasers, but they tilt the odds toward steadier days and gentler recoveries.
Conclusion: Build Your Personalized, Natural Migraine Plan
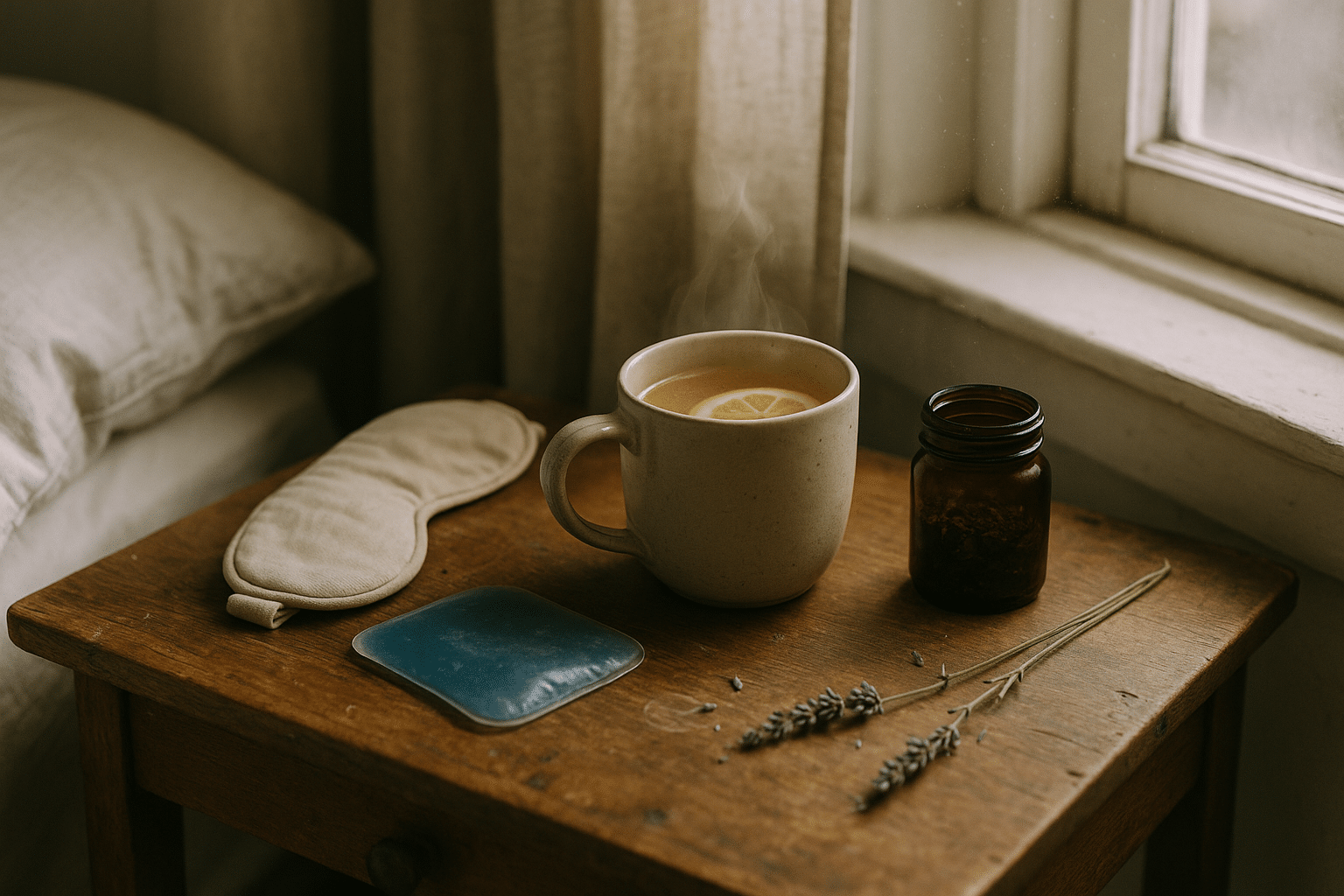
You now have a toolkit that ranges from quick comforts to long-game prevention. The art is personalizing it. Start by mapping your triggers for two to four weeks, then choose one foundation to strengthen—often sleep timing or meal regularity—before layering in others. Next, assemble a small acute-care kit: a flexible cold pack, earplugs or an eye mask, a sealed bottle for water and electrolytes, ginger tea or capsules, and a diluted peppermint or menthol balm. Place it where you can reach it quickly, and practice using it at the first whisper of symptoms.
Draft a simple plan you can test and refine:
– Daily: consistent sleep window, 2–3 liters of fluids, regular meals with protein and fiber, and 20–40 minutes of gentle movement
– Preventive: consider magnesium or riboflavin if appropriate, reviewing dose and interactions with your clinician
– Acute: dark room, cold pack, hydration, ginger, and (if you tolerate it) a small early caffeine dose
– Regulation: two to three micro-sessions of breathwork or mindfulness every day
Safety matters. Seek urgent medical attention for new, sudden, “worst-ever” headaches, changes in neurological function (weakness, confusion, fainting), fever and neck stiffness, head injury, or headache beginning after age 50. If you are pregnant, planning pregnancy, or nursing, review all supplements and herbs with a professional. Natural does not always mean risk-free, and the goal is to complement—not replace—careful medical guidance when needed.
With migraines, progress often looks like fewer severe days, faster recovery after flares, and a bit more confidence navigating triggers. Celebrate those wins. Your plan will evolve with the seasons of your life; keep notes, stay curious, and prioritize consistency over intensity. And if this guide helps you reclaim even one afternoon each week, that momentum is worth protecting. Be patient with the process—relief is rarely a single leap, but a steady walk on a path you now know how to find.


